
What is glycemic index? The role of index and glycemic load in diabetes
The level of blood glucose is influenced by both the amount of carbohydrates consumed and their type, and that’s where…
Type 1 diabetes is called in Latin: Diabetes mellitus typi 1, previously described as Insulin Dependent Diabetes Mellitus, or IDDM). This disease is an autoimmune condition, i.e. the body destroys its own cells. As a consequence of this process, insulin-producing beta islet cells are completely destroyed. The end result is a loss of the ability of the pancreas to produce insulin. The only effective treatment for this type of diabetes is administration of insulin by subcutaneous injection or continuous subcutaneous insulin infusion using an insulin pump (1).

You may have wondered if your type of diabetes is the same as your grandmother’s or your neighbor’s. This is not necessarily the case, because diabetes can have many varieties. The main difference between type 1 and type 2 diabetes is the inability to secrete insulin in type 1. On the other hand, type 2 is dominated by insulin resistance, which means that pancreas can produce insulin, but the body is unable to use it properly, usually due to excess body fat.
In type 1 diabetes, the onset of the disease is usually quite fast and intensive. Therefore, it is really difficult to overlook the accompanying symptoms. The clinical manifestations of type 1 diabetes are quite characteristic, and the most common ones include:

Due to the fact that type 1 diabetes develops at a fairly rapid pace and the symptoms are quite acute, the patient often has to be hospitalized (preferably in a recommended center that specializes in the treatment of type 1 diabetes). Only after achieving glucose leveling and going through the education process can they be discharged home and continue to cope on their own in this new situation.
The first question that many patients ask immediately after hearing the diagnosis is: where did diabetes come from, and why me? It is difficult to give just one answer because there is no single cause for the disease.
One thing is certain: no patient with type 1 diabetes had an effect on its occurrence because this disease appears completely independent of their actions. The only thing you can influence is how your disease will go on and how you will treat it.
The mechanism that leads to the development of type 1 diabetes is the autoimmune process. The body produces autoantibodies that lead to the destruction of beta cells in the pancreas, and ultimately to absolute insulin deficiency. Diabetes occurs when 90% of the insulin-producing cells are destroyed. There is no consensus among scientists as to the predominance of genetic or environmental factors conducive to the development of diabetes. Some tendency to develop diabetes is inherited, and HLA genes seem to be playing a crucial role here.
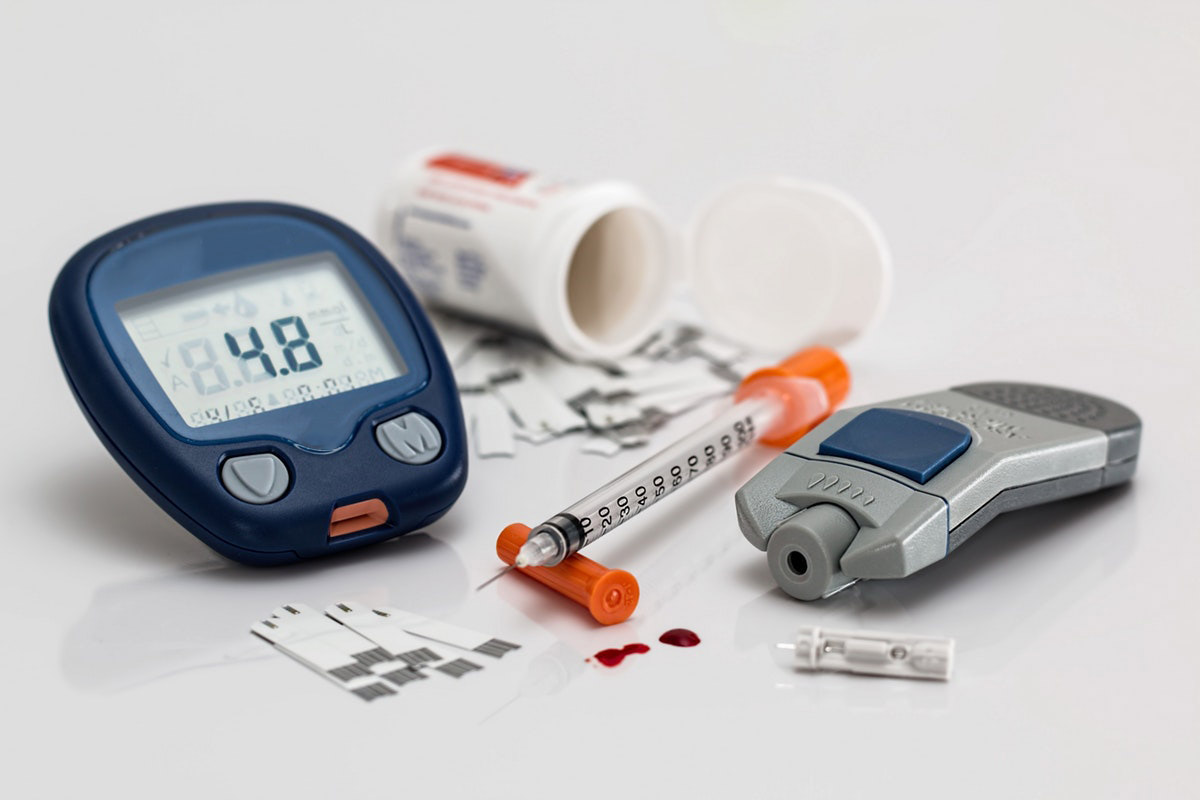
In type 1 diabetes, because of the deficiency of insulin, the only way to supplement this hormone is to provide it to the body. Currently, the only effective way to administer insulin is by subcutaneous injection. The most effective and recommended model for the treatment of type 1 diabetes is intensive functional insulin therapy. It is a method that mimics the action of the pancreas in a healthy person.
In a healthy person, the pancreas secretes small doses of insulin throughout the day to maintain adequate glucose levels in the body. When you eat a meal, it produces much more to control your blood glucose (blood glucose). The method of intensive insulin therapy works in the same way, except that the patient thinks for his/her pancreas and decides what dose of insulin to give. Your basal insulin dose (which works throughout the day) is determined by your doctor. On the other hand, doses of meal-related insulin are calculated by the patient, depending on how much he wants to eat and what it will be. This method involves repeated insulin administration throughout the day, or a continuous subcutaneous infusion using a personal insulin pump (2).

 Read more
Read more

The level of blood glucose is influenced by both the amount of carbohydrates consumed and their type, and that’s where…

Metabolic control of diabetes is influenced not only by the treatment method and lifestyle changes, but also by the patient’s…

What causes type 2 diabetes Diabetes belongs to the group of metabolic diseases characterized by hyperglycemia, i.e. too high blood…

Diet for diabetes – what to eat and what to avoid in diabetes The treatment of diabetes should be comprehensive…

Cukrzyca ciążowa (ang. Gestational Diabetes Mellitus – GDM) jest najczęstszym powikłaniem metabolicznym występującym u kobiet ciężarnych.

It has been assumed that glycemic index (GI) for glucose is 100 and other products refer to this value. It…
